Delayed Sequence Intubation
Delayed Sequence Intubation (DSI)
General Concepts
- DSI is procedural sedation/dissociation where the procedure is preoxygenation
- Breaks up the sequence of RSI to preoxygenate prior to paralysis—prolongs safe apnea duration and decreases risk of gastric insufflation or aspiration
- Maintains patient’s spontaneous respirations and reflexes
Candidates for DSI
- Agitated due to EtOH, head injury, or psychosis, but with normal lungs
- Agitated, but with lungs capable of being oxygenated on non-rebreather (NRB) mask: hypoxic due to COPD, pneumonia, ARDS
- Agitated, but require non-invasive positive pressure ventilation (NIPPV) to preoxygenate
- Unobtainable or unacceptable vital signs due to any of the above
- Need to perform a procedure that the patient is not tolerating prior to intubation (e.g. NGT placement prior to intubation of GI bleeder)
Ketamine
- Dose: 1 mg/kg IV push (may need to re-dose 0.5 mg/kg to maintain dissociation)
- Pros: 30 sec onset, achieves dissociative state, maintains spontaneous respirations and airway reflexes, maintains hemodynamic stability
- Cons: May increase intracranial pressure in patients with high MAP, may cause laryngospasm, use with caution in patients with CAD, HTN, or tachycardia
Equipment and Troubleshooting
- Respiratory therapist
- Nasal cannula (NC)
- Non-rebreather (NRB) mask
- Bag valve mask (BVM) with PEEP valve
- 2 O2 flow meters (NRB or BVM, NC)
- Ventilator with NIPPV settings
- Non-vented mask with straps for CPAP
- End tidal CO2 monitor
Pearls: DSI ≠ NIV
- Preoxygenation may be achieved with NC, NRB mask, OR NIPPV, depending on the patient’s needs
- If your patient is not agitated, NIV may be sufficient without the need for sedation/dissociation
- Intubation may be avoided if adequate dissociation and oxygenation is attained
Delayed Sequence Intubation (DSI) algorithm
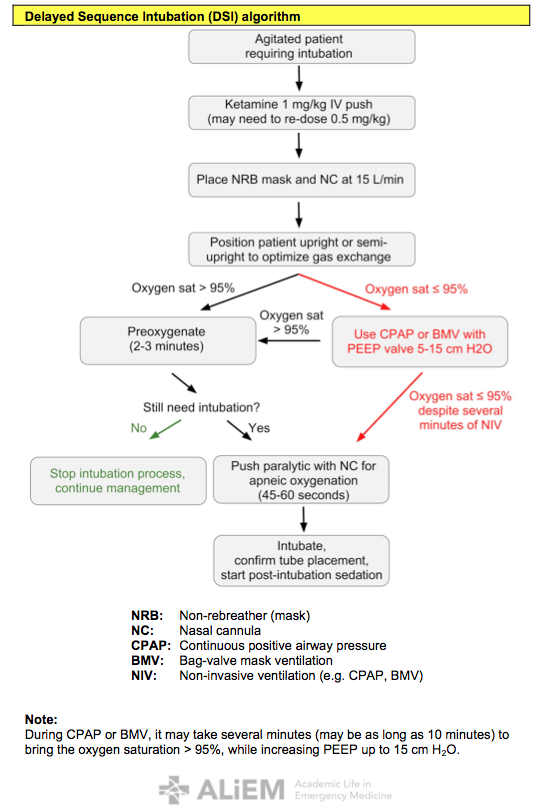
Note: During CPAP or BMV, it may take several minutes (may be as long as 10 minutes) to bring the oxygen saturation > 95%, while increasing PEEP up to 15 cm H2O.
References
- Weingart SD. Preoxygenation, reoxygenation, and delayed sequence intubation in the emergency department.J Emerg Med. 2011 Jun;40(6):661-7. doi: 10.1016/j.jemermed.2010.02.014. Epub 2010 Apr 8. [PubMed]
- Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012 Mar;59(3):165-75.e1. doi: 10.1016/j.annemergmed.2011.10.002. Epub 2011 Nov 3 [PubMed]
- Sehdev RS, Symmons DA, Kindl K. Ketamine for rapid sequence induction in patients with head injury in the emergency department. Emerg Med Australas. 2006 Feb;18(1):37-44. [PubMed]
- Bourgoin A, Albanèse J, Wereszczynski N, Charbit M, Vialet R, Martin C.Safety of sedation with ketamine in severe head injury patients: comparison with sufentanil.Crit Care Med. 2003 Mar;31(3):711-7. [PubMed]
- Weingart SD, Trueger NS, Wong N, Scofi J, Singh N, Rudolph SS. Delayed Sequence Intubation: A Prospective Observational Study. Ann Emerg Med. 2015 Apr;65(4):349-55. doi: 10.1016/j.annemergmed.2014.09.025. Epub 2014 Oct 23. [PubMed]