Ventilator Setting for Lung Protection
Ventilator Setting for Lung Protection
Lung protection: Strategy for patients with lung injury and those prone to lung injury. This applies to every intubated patient except those with acute asthma/COPD.
Initial ventilator setting for patient with predicted body wt = 70 kg (5'9" male; 5'11" female)
|
|
Ventilator Mode
Volume Assist Control (AC)
Tidal Volume (Vt)
6-8 mL/kg (LUNG PROTECTION)
- Based on predicted body weight (kg)
- If acute lung injury (ALI) or ARDS present, goal is to bring down to 6 mL/kg
- Do NOT alter to fix ventilation, but may need to alter if plateau pressure is > 30 cmH2O, see below). Only protects lung by preventing barotrauma.
Inspiratory Flow Rate (IFR)
60-80 L/min (PATIENT COMFORT)
- Increase IFR and ensure adequate sedation if patient uncomfortable or sucking on tube
Respiratory rate (RR)
Start at 16-18, then adjust based on pCO2 (VENTILATION)
- Goal pH = 7.30 - 7.45
- Goal pCO2 = mild hypercarbia
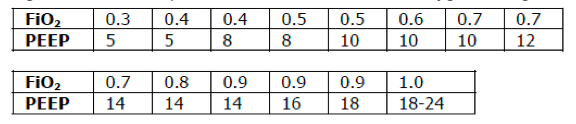
FiO2 & PEEP
Start at FiO2 100% and PEEP 5 (OXYGENATION)
- Goal PaO2=55-80 or SpO2=88-95%
- Wait 5-15 min, then draw an ABG
- If ABG and SpO2 show adequate oxygenation, drop FiO2 to 30-40% and begin titrating FiO2 and PEEP per the chart below to achieve oxygenation goal.
Plateau Pressure (Pplt)
- Goal Pplt <30 cmH2O
- Check after initial settings, and at regular intervals thereafter
- Technique: Press inspiratory hold button for 0.5 sec and look at pressure gauge
- If Pplt >30 cmH2O, lower Vt until you acheive your goal
- May need to go as low as 4 mL/kg of predicted body weight
References
- NHLBI ARDS Network, "Ventilator Protocol Card" [Source]
- Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000 May 4;342(18):1301-8. [PubMed]